
I’m currently taking a short break from the blog, but encourage you to follow along on Instagram. I will be back with blog content soon. To know exactly when that happens, make sure to subscribe!
Thanks and ‘see’ you soon!


I’m currently taking a short break from the blog, but encourage you to follow along on Instagram. I will be back with blog content soon. To know exactly when that happens, make sure to subscribe!
Thanks and ‘see’ you soon!

This week, we learned of the passing of beloved Chadwick Boseman, known for his role in movies such as Black Panter, 42, Marshall, Da 5 Bloods, and many others. I personally learned that in recent months, Chadwick had been bullied on social media for his gaunt appearance. Little did many know, Chadwick was sick. He had been diagnosed with colon cancer stage 3 in 2016, which had progressed to stage 4. He died August 28th, 2020. His weight loss was in fact a consequence of his illness. Before you comment on people’s weight loss, realize that it may be completely unintentional; you never know what people are going through behind the scenes.
Did you know that colon cancer – also known as colorectal cancer – excluding skin cancers, is the third most common cancer diagnosed in both men and women in the United States. There are major health disparities in colon cancer incidence, with non-Hispanic Black individuals experiencing far greater rates of colon cancer than other racial ethnic groups.
“During 2009-2013, CRC incidence rates in
blacks were about 20% higher than those in non-Hispanic
whites (NHWs) and 50% higher than those in APIs. The
disparity for mortality is twice that for incidence; CRC death
rates in blacks are 40% higher than in NHWs and double
those in APIs. Reasons for racial/ethnic disparities in CRC
are complex, but largely reflect differences in socioeconomic
status. According to the US Census Bureau, 24% of blacks
lived in poverty in 2015, compared to 11% of Asians and 9%
of NHWs. People with the least education (used in studies
to estimate socioeconomic status) are 40% more likely to be
diagnosed with CRC than those with the most education.
Close to half (44%) of the socioeconomic disparity is
attributed to differences in the prevalence of behavioral
factors associated with CRC (e.g., smoking, obesity). (See
page 11 for information on risk factors for CRC.) A similar
proportion (42%) of the racial disparity in incidence is
estimated to be due to differences in CRC screening, which
combined with lower stage-specific survival accounts for
about half of the racial disparity in CRC mortality.”

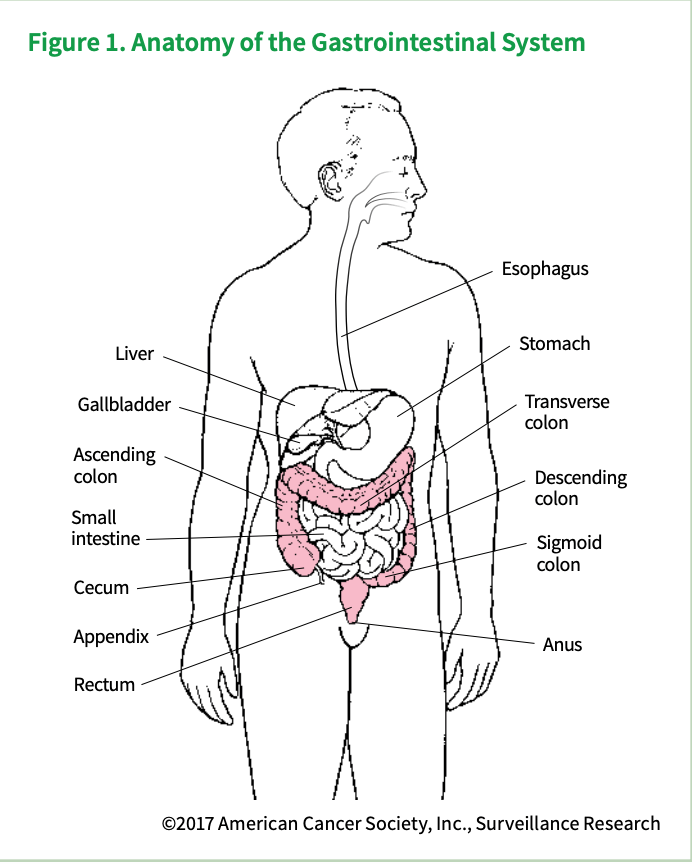
What is colorectal cancer?
Colorectal cancer often begins as a growth called a polyp inside the colon or rectum. Finding and removing polyps can prevent colorectal cancer. Some cancers start in the colon and others start in the rectum. The majority occur in the colon.
The following information is from the Mayo Clinic. Additional information can be found here: https://www.mayoclinic.org/diseases-conditions/colon-cancer/symptoms-causes/syc-20353669
Signs and symptoms of colon cancer include:
Doctors aren’t certain what causes most colon cancers.
In general, colon cancer begins when healthy cells in the colon develop changes (mutations) in their DNA. A cell’s DNA contains a set of instructions that tell a cell what to do.
Healthy cells grow and divide in an orderly way to keep your body functioning normally. But when a cell’s DNA is damaged and becomes cancerous, cells continue to divide — even when new cells aren’t needed. As the cells accumulate, they form a tumor.
With time, the cancer cells can grow to invade and destroy normal tissue nearby. And cancerous cells can travel to other parts of the body to form deposits there (metastasis).
Factors that may increase your risk of colon cancer include:
Doctors recommend that people with an average risk of colon cancer consider colon cancer screening around age 50. But people with an increased risk, such as those with a family history of colon cancer, should consider screening sooner.
Several screening options exist — each with its own benefits and drawbacks. Talk about your options with your doctor, and together you can decide which tests are appropriate for you.
You can take steps to reduce your risk of colon cancer by making changes in your everyday life. Take steps to:
Some medications have been found to reduce the risk of precancerous polyps or colon cancer. For instance, some evidence links a reduced risk of polyps and colon cancer to regular use of aspirin or aspirin-like drugs. But it’s not clear what dose and what length of time would be needed to reduce the risk of colon cancer. Taking aspirin daily has some risks, including gastrointestinal bleeding and ulcers.
These options are generally reserved for people with a high risk of colon cancer. There isn’t enough evidence to recommend these medications to people who have an average risk of colon cancer.
If you have an increased risk of colon cancer, discuss your risk factors with your doctor to determine whether preventive medications are safe for you.”
Colorectal cancer can be treated and survival rates are high if caught early. I realize many are worried about health checks during the COVID pandemic, but if you are due for a check or have any of the symptoms mentioned above, make sure you don’t delay those health checks.

One of my favorite things to do all year is watch my boys play rec little league baseball. They love it, they’re good at it, they have fun, and overall it’s a great way to get some physical activity and socialization in.
A lot changed when COVID-19 became a worry in our lives five months ago. One of the thing that changed the most for my kids – and other kids across the US – was that they were unable to play baseball for some time. While little league baseball did eventually resume, we opted out for the remaining of the season this summer. The main reason: I wanted to see what safety measures were going to be put into place, considering local numbers.
As we contemplate a return this fall, I wondered, what are the recommendations for a return to play? While the NCAA has issued guidance for collegiate sports, less was known about what recreational leagues should do to safely resume play. Several teams across the US reported cases among kids and coaches, both in rec leagues of all ages (eg, here, here, and here to list a few) and in collegiate sports. Unfortunately, no teams at the recreational level are implementing sentinel testing, so teams have to rely on self-report of covid-positive status and or symptoms. We know now that kids of all ages are susceptible to covid, but can also transmit it, but most importantly, that asymptomatic spread is a major concern for COVID-19.
All summer I looked for guidance, only to find very limited information about what should and should not happen upon resumption to play. Luckily, a league from Mercer Island (MI) in Washington State came up with some guidance that has since been adapted by the national Little League organization. Two main documents you should read (and share with your local leagues) are:
Best Practices for Creating a Local Little League® Social Distancing Plan
and
Mercer Island Little League Social Distancing Plan
Among the main points:
We all want life to return to normal. Recreational sports brings communities together, but can also be a source of infection if people are not careful. Proper safety regulations are therefore necessary to avoid further spread of COVID-19, especially in states where case numbers remain high. To engage in activities like outdoor sports like little league baseball while implementing harm reduction strategies, for example, you must:
2. Avoid close contact: doable with physical distancing.
3. Avoid closed spaces: sports is outdoors, but you have to worry about and try to avoid bathrooms, carpools, press boxes, dugouts (especially non-well ventilated ones), indoor dining after sports, and concession stands (if any are indoors, but especially for workers).
4. Wash your hands frequently: Hard to do in park bathrooms safely, so consider having hand sanitizer available.
5. Wear your mask: Especially when 6′ distance between players/spectators/coaches, etc cannot be maintained.
6. Watch your distance: Physical distancing between all individuals at the park is essential, especially between people who are not from the same household.