
This is me, giving an interview – non COVID-19 related though… 🙂
I know this post is coming late tonight, but hopefully you will read it first thing Monday morning, and hopefully it will help answer some of the questions you might have about COVID-19, formerly known as “2019-N Cov Virus”. A few weeks ago, I wrote a post all what we knew then (if you haven’t read it, brush up here), but we have learned a lot about it since I wrote that post. Buckle up, there are a number of things to keep in mind below.
1) The Media and Scientists
First, let me be clear. There are two wars we are fighting in this moment: 1) the fight to stop the spread of COVID-19 and 2) the fight to combat misinformation. Many scientists are actively working to gather as much evidence-based information as possible and subsequently share it with the public as quickly and accurately as possible. This is happening in the form of press conferences, social media posts, newspaper articles, etc. If you happen to read or hear something about COVID-19, be assured that it is coming from a reliable source. Information from the Centers for Disease Control, the World Health Organization, the National Institutes of Health (yes, especially Dr. Anthony Fauci), heads of local health departments – all reliable sources that you can count on to have reliable, not overly exaggerated or inaccurate information. My colleague Dr. Ellie Murray curated a list of trusted scientists who are sharing information on Twitter. She shared it with me here if you’re interested. Lots of other trusted sources you can follow on that thread. Yes, this – like many other situations – has become highly politicized and there are media outlets and businesses that will benefit from headlines and tag-lines that cause fear. Let me ask you this: When is panicking ever a good idea? NEVER. Probably not unless a lion is chasing you through the savanna and honestly, how many times is that going to happen in your life, really? So, take a pause, think critically, and double check the information you hear or read about by going to one of the sources I named previously. If you ever have additional questions that can’t be answered there, please feel free to email me or send me a DM on Instagram.
2) Don’t Panic
While we’re on the topic of panicking though, it would be insensitive of me to tell you not to panic when you have clearly heard that there have been deaths associated with COVID-19, including one to date in the US. Especially if you have loved ones who fall in these age categories or may simply more likely to get pretty sick with any viral infection. The data suggests that deaths have occurred as a result of infection with COVID-19, affecting some age groups more than other. According to reports:
- 14.8% of deaths among people known to have COVID-19 aged >80 years of age
- 8% of deaths among people known to have COVID-19 aged 70-79 years
- 3.6% of deaths among people known to have COVID-19 aged 60-69 years of age
- 2.3% of deaths among people known to have COVID-19 aged 10-59 years of age
As you can see, the biggest risk seems to be for people in the older age groups. As mentioned in my original post and my flu post, people with weakened immune systems, COPD, and other conditions that may them get pneumonia more easily, are likely to get pretty sick if infected with COVID-19 too. It’s important to note that these are percentages based on known cases. We don’t really know how many people are infected overall, so these percentages are just estimates. The number of total cases and deaths do still remain lower than the total number of cases and deaths due to flu. That said, still important to treat this epidemic with seriousness and try to…
3) Prevent the spread
Okay, so if I’m telling you not to panic, then why shouldn’t we panic and what should we do instead? Well, for starters, you should do what you should be doing even in the absence of COVID-19:
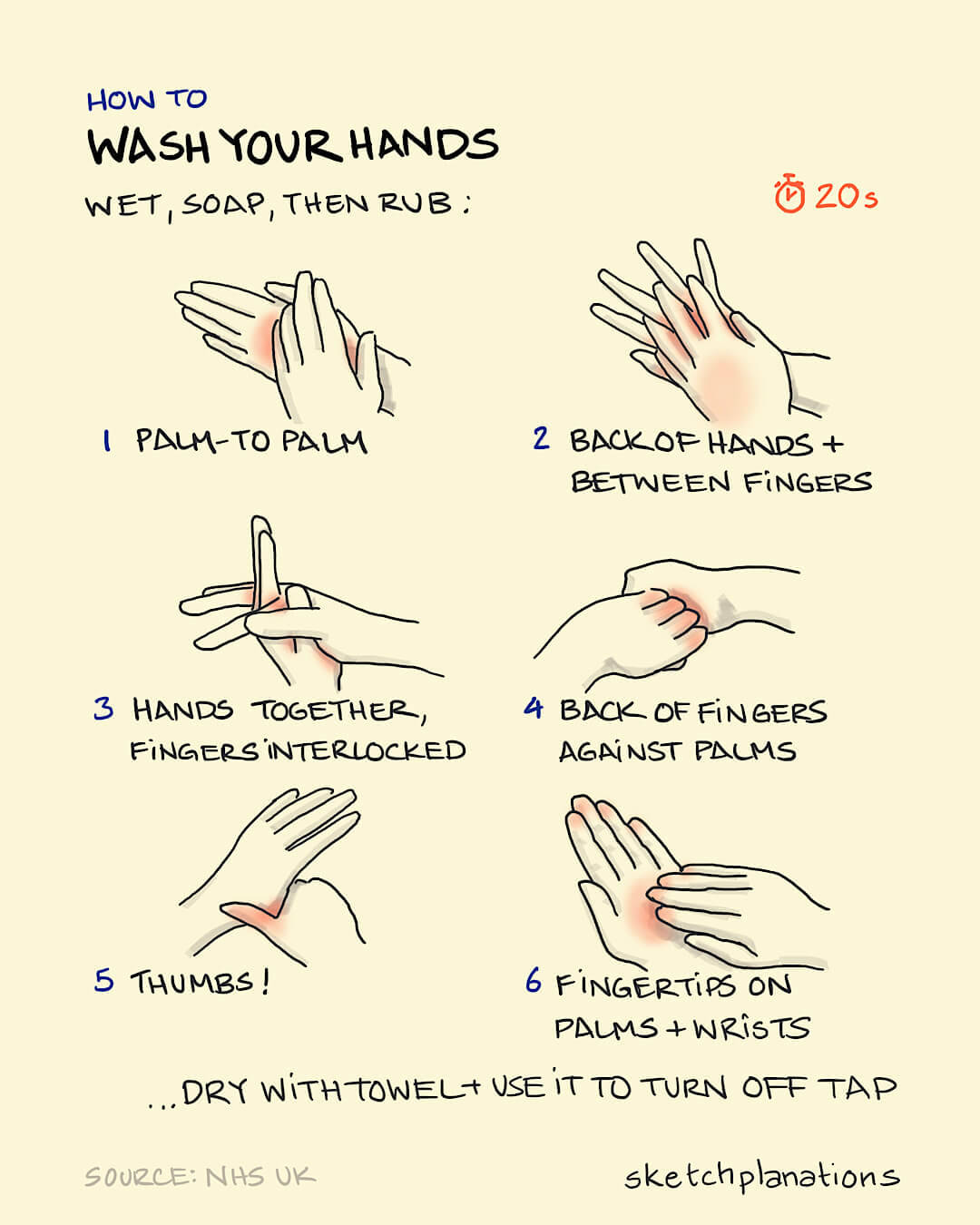
- WASH YO HANDS!
- COVER YO MOUTH WHEN YOU COUGH
- STAY HOME WHEN YOU’RE SICK – I recognize this is hard for those who do not have flexible jobs, so as best as you can, please try not to be around other people when you are feverish and sickly.
Sorry, was that too shouty?? Yikes. #sorrynotsorry Seriously, friends. These tried and true measures will do a lot to help prevent the spread of COVID-19, BUT ALSO, the flu, the common cold, strep throat, pink eye, I mean…the list is kinda endless!
Practicing good respiratory hygiene is so important. Also important to keep in mind is to try and avoid touching your eyes, nose, or mouth as much as possible. That’s so that if you happened to not wash your hands well enough (more on that below), you will lower the chances of transferring any virus on your hand into the parts of your face where the virus can enter your body. It’s obvi more complicated than that, but you get the message – I hope!
4) Prepare
Okay, fine. So, what if I do all those things but I hear that the numbers of cases are still increasing?? Well, chances are that you will likely see the number of cases increase FO SHO. Why? Because it’s part of the natural process of identifying new people with the infection, especially when we don’t yet have a good way to screen for COVID-19 like we do with the flu or strep throat for example. So, if there happen to be more cases – and there will – and if there happen to be school or workplace closures (and there might), keep a few things in mind, just as you would for your regular preparedness plan – because you have one, RIGHT??!
- Do NOT buy a mask. If you are healthy, you do not need a mask. Most masks require fit-testing in order to be truly effective. No need to spend your money on that. Buy some mascara or extra deodorant. I promise.
- If you simply MUST buy something, buy what you would for the flu or cold: decongestants, anti-inflammatory drugs and acetaminophen for fevers.
- Have non-perishables on hand like canned goods, water, toilet paper, etc in case there are any closures and/or if you happen to be sick and cannot get to the store. This is always good to keep on hand though, so a good plan regardless.
- In general, it’s good to have a preparedness plan that can apply to any situtation. You can find a good one provided by the CDC here: https://www.cdc.gov/ncbddd/hemophilia/documents/familyemergencykitchecklist.pdf
5) Be a good citizen
This is a lot of information, and honestly, there are a lot of details about COVID-19 that I didn’t include here. But honestly, based on what we know currently, this is as much as I thought was worth sharing. The situation is changing very rapidly and we still don’t fully understand what things will look like here in the US. We still don’t have a gold standard for screening for COVID-19 nor do we have a tried and tested treatment, though there are treatment recommendations should you test positive and need to be treated.
What I do want to emphasize is that in order to prevent further spread in the US and to come out of all of this in the best way possible, it’s so very important that we all be good citizens. What does that mean? Do all the things I mentioned above to the best of your ability, and don’t let fear get the best of you. There are so many reports out there of prejudice and discrimination against certain groups and populations since news of COVID-19 began to circulate. If you want to blame someone, blame the virus. Don’t blame your neighbors. Deal?
Information for this post came from:
https://www.theatlantic.com/health/archive/2020/02/covid-vaccine/607000/
https://www.popsci.com/story/health/how-diseases-spread/
https://jamanetwork.com/journals/jama/fullarticle/2760782#.Xlqw4Q2V-iY.twitter (especially good read for clinicians)
https://www.sketchplanations.com/post/611288424379449344/how-to-wash-your-hands-in-these-times-and-to-be (with wonderful infographics like the one below)
The Centers for Disease Control
World Health Organization
National Institutes of Health

